Overview
-
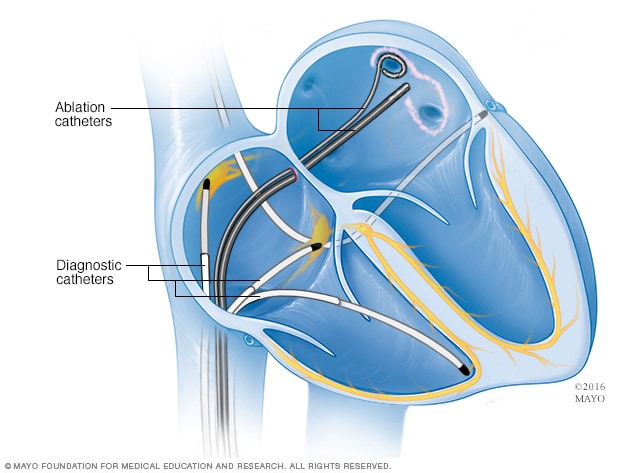
Cardiac ablation
Cardiac ablation
Cardiac ablation is a procedure to scar or destroy tissue in your heart that's allowing incorrect electrical signals to cause an abnormal heart rhythm. Diagnostic catheters are threaded through blood vessels to your heart where they are used to map your heart's electrical signals. Ablation catheters transmit heat or cold to scar or destroy tissue. This illustration shows ablation catheters being applied near the pulmonary veins in a type of cardiac ablation called pulmonary vein isolation.
Cardiac ablation works by scarring or destroying tissue in your heart that triggers or sustains an abnormal heart rhythm. In some cases, cardiac ablation prevents abnormal electrical signals from entering your heart and, thus, stops the arrhythmia.
Cardiac ablation is sometimes done through open-heart surgery, but it's often done using catheters, making the procedure less invasive and shortening recovery times.
Types
- Atrial flutter ablation
- Pulmonary vein isolation
- SVT ablation
- Ventricular tachycardia ablation
Why it's done
Cardiac ablation is a procedure that's used to correct heart rhythm problems.When your heart beats, the electrical impulses that cause it to contract must follow a precise pathway through your heart. Any interruption in these impulses can cause an abnormal heartbeat (arrhythmia), which can sometimes be treated with cardiac ablation.
Ablation isn't usually your first treatment option. Ablation is a treatment option for people who:
- Have tried medications to treat an arrhythmia without success
- Have had serious side effects from medications to treat arrhythmias
- Have certain types of arrhythmias that respond well to ablation, such as Wolff-Parkinson-White syndrome and supraventricular tachycardia
- Have a high risk of complications from their arrhythmias, such as sudden cardiac arrest
Risks
Cardiac ablation carries a risk of complications, including:- Bleeding or infection at the site where your catheter was inserted
- Damage to your blood vessels where the catheter may have scraped as it traveled to your heart
- Puncture of your heart
- Damage to your heart valves
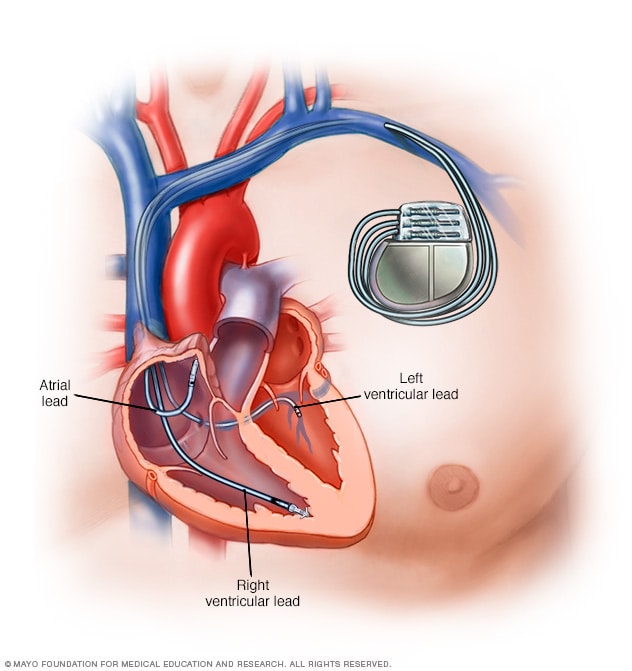
- Damage to your heart's electrical system, which could worsen your arrhythmia and require a pacemaker to correct
- Blood clots in your legs or lungs (venous thromboembolism)
- Stroke or heart attack
- Narrowing of the veins that carry blood between your lungs and heart (pulmonary vein stenosis)
- Damage to your kidneys from dye used during the procedure
- Death in rare cases
How you prepare
Your doctor will evaluate you and may order several tests to evaluate your heart condition. Your doctor will discuss with you the risks and benefits of cardiac ablation.You'll need to stop eating and drinking the night before your procedure. If you take any medications, ask your doctor if you should continue taking them before your procedure.
Your doctor will let you know if you need to follow any other special instructions before or after your procedure. In some cases, you'll be instructed to stop taking medications to treat a heart arrhythmia several days before your procedure.
If you have an implanted heart device, such as a pacemaker or implantable cardioverter-defibrillator, talk to your doctor to see if you need to take any special precautions.
What you can expect
During cardiac ablation
-
Catheter insertion points for cardiac ablation
Catheter insertion points for cardiac ablation
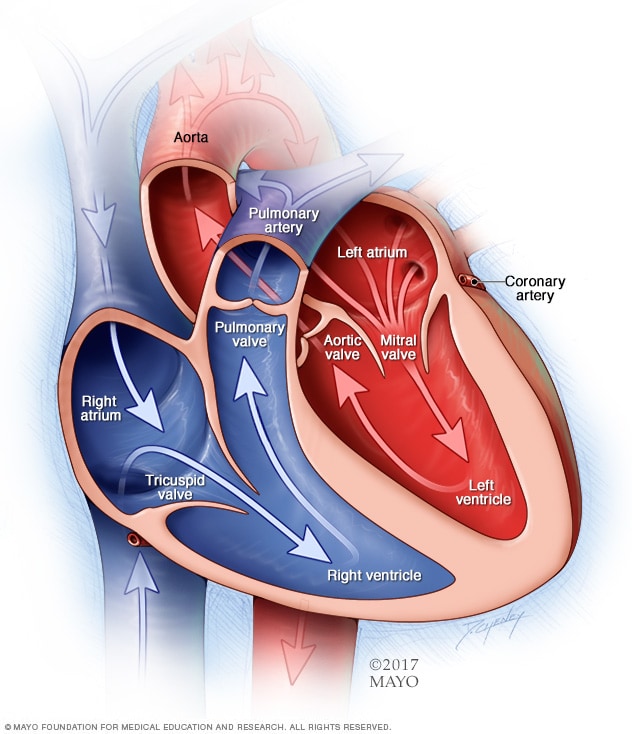
During cardiac ablation, catheters are passed through a vein in order to reach your heart. Catheters may be inserted in your groin, your shoulder or your neck.
After your sedative takes effect, your doctor or another specialist will numb a small area near a vein on your groin, neck or forearm. Your doctor will insert a needle into the vein and place a tube (sheath) through the needle.
Your doctor will thread catheters through the sheath and guide them to several places within your heart. Your doctor may inject dye into the catheter, which helps your care team see your blood vessels and heart using X-ray imaging. The catheters have electrodes at the tips that can be used to send electrical impulses to your heart and record your heart's electrical activity.
This process of using imaging and other tests to determine what's causing your arrhythmia is called an electrophysiology (EP) study. An EP study is usually done before cardiac ablation in order to determine the most effective way to treat your arrhythmia.
Once the abnormal heart tissue that's causing the arrhythmia is identified, your doctor will aim the catheter tips at the area of abnormal heart tissue. Energy will travel through the catheter tips to create a scar or destroy the tissue that triggers your arrhythmia.
In some cases, ablation blocks the electrical signals traveling through your heart to stop the abnormal rhythm and allow signals to travel over a normal pathway instead.
The energy used in your procedure can come from:
- Extreme cold (cryoablation)
- Heat (radiofrequency)
- Lasers
During the procedure, it's possible you'll feel some minor discomfort when the catheter is moved in your heart and when energy is being delivered. If you experience any type of severe pain or shortness of breath, let your doctor know.
After cardiac ablation
Following your procedure, you'll be moved to a recovery area to rest quietly for four to six hours to prevent bleeding at your catheter site. Your heartbeat and blood pressure will be monitored continuously to check for complications of the procedure.Depending on your condition, you may be able to go home the same day as your procedure, or you may need to stay in the hospital. If you go home the same day, plan to have someone else drive you home after your procedure.
You may feel a little sore after your procedure, but the soreness shouldn't last more than a week. You'll usually be able to return to your normal activities within a few days after having cardiac ablation.
Results
Although cardiac ablation can be successful, some people need repeat procedures. You may also need to take medications, even after you've had ablation.To keep your heart healthy, you may need to make lifestyle changes that improve the overall health of your heart, especially to prevent or treat conditions that can cause or worsen arrhythmias, such as high blood pressure. Your doctor may suggest that you:
- Use less salt, which can help lower blood pressure
- Increase your physical activity
- Quit smoking
- Avoid drinking alcohol
- Eat heart-healthy foods
- Maintain a healthy weight
- Manage strong emotions, such as anger