Overview
A pacemaker is a small device with two parts — a generator and wires (leads, or electrodes) — that's placed under the skin in your chest to help control your heartbeat.People may need a pacemaker for a variety of reasons — mostly due to one of a group of conditions called arrhythmias, in which the heart's rhythm is abnormal.
Some medications can affect your heart rate as well. For some, genetic conditions cause an abnormal heart rate. Regardless of the underlying cause of an abnormal heart rate, a pacemaker may fix it.
A pacemaker can often be implanted in your chest with a minor surgery. You may need to take some precautions in your daily life after your pacemaker is installed.
Mayo Clinic's approach
Types
Why it's done
-
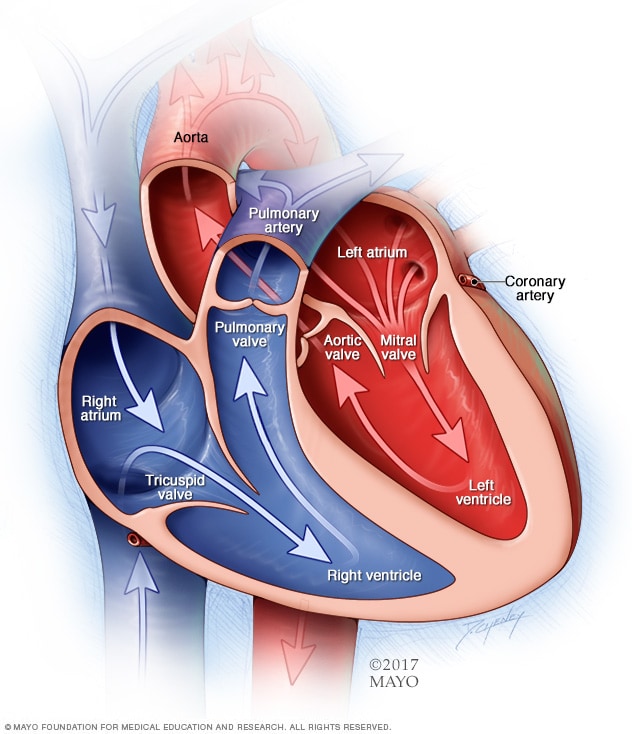
Chambers and valves of the heart
Chambers and valves of the heart
A normal heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of your heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
-
The conduction system
The conduction system
Your heart's natural pacemaker — the sinus node — produces electrical impulses that prompt your heart to beat.
-
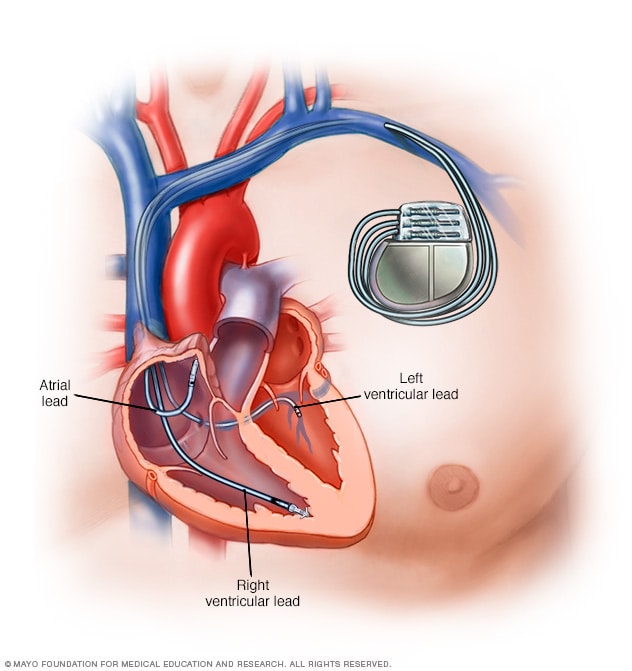
Pacemaker
Pacemaker
Your heart's natural pacemaker — the sinus node — produces electrical impulses to stimulate your heart to beat. If these impulses are disrupted, you may need an artificial pacemaker. Depending on your condition, you may have a pacemaker with one to three flexible, insulated wires (leads) placed in a chamber, or chambers, of your heart. These wires deliver the electrical pulses to adjust your heart rate.
Pacemakers can also be implanted permanently to correct a slow heartbeat (bradycardia) or, in some cases, to help treat heart failure.
Smaller pacemakers about the size of a pill have been developed and are currently undergoing clinical trials. This new, leadless device can be implanted directly into the heart, where it emits an electrical impulse to control the heartbeat. Because a lead isn't required, this device can minimize the risk of infection and speed recovery time.
How your heart beats
To understand how a pacemaker works, it helps to know how your heart beats.The heart is a muscular, fist-sized pump with four chambers, two on the left side and two on the right. The upper chambers are the right and left atria. The lower chambers are the right and left ventricles.
For your heart to function properly, the heart's chambers must work in a coordinated fashion. Your heart must also beat at an appropriate rate — normally from 60 to 100 beats a minute in resting adults. If your heart beats too slowly or too rapidly, not enough blood flows through your body, leading to fatigue, fainting, shortness of breath, confusion, and other signs and symptoms.
Your heart's electrical system controls the chambers' pumping action. A normal heartbeat begins in your right atrium, in the sinus node. This cluster of cells — your natural pacemaker — acts like a spark plug, generating regular electrical impulses that travel through specialized muscle fibers.
When an electrical impulse reaches both the right and left atria, they contract and squeeze blood into the ventricles. After a split-second delay to allow the ventricles to fill, the impulse reaches the ventricles, making them contract and pump blood to the rest of your body.
What a pacemaker does
An implanted electronic pacemaker mimics the action of your natural pacemaker. An implanted pacemaker consists of two parts:- The pulse generator. This small metal container houses a battery and the electrical circuitry that regulates the rate of electrical pulses sent to your heart.
- Leads (electrodes). One to three flexible, insulated wires are each placed in a chamber, or chambers, of your heart and deliver the electrical pulses to adjust your heart rate.
Single chamber pacemaker
This type of pacemaker usually carries electrical impulses from the pulse generator to the right ventricle of your heart.Dual chamber pacemaker
A dual chamber pacemaker carries electrical impulses from the pulse generator to both the right ventricle and the right atrium of your heart. The impulses help control the timing of contractions between the two chambers.Biventricular pacemaker
A biventricular pacemaker is a treatment option for people with heart failure whose hearts' electrical systems have been damaged. Unlike a regular pacemaker, a biventricular pacemaker stimulates both of the lower chambers of the heart (the right and left ventricles) to make the heart beat more efficiently.A biventricular pacemaker paces both ventricles so that all or most of the ventricular muscle pumps together. This allows your heart to pump blood more effectively. Because this treatment resets the ventricles' pumping mechanism, it's also referred to as cardiac resynchronization therapy (CRT).
Risks
Complications from having surgery to implant your pacemaker are uncommon, but could include:- Infection where the pacemaker was implanted
- Allergic reaction to the dye or anesthesia used during your procedure
- Swelling, bruising or bleeding at the generator site, especially if you are taking blood thinners
- Damage to your blood vessels or nerves near the pacemaker
- Collapsed lung
How you prepare
Before your doctor decides if you need a pacemaker, you'll have several tests done to find out the cause of your irregular heartbeat. These could include:- Electrocardiogram. In this noninvasive test, sensor pads with wires attached, called electrodes, are placed on your chest and sometimes your limbs to measure your heart's electrical impulses. Your heart's beating pattern can offer clues to the type of irregular heartbeat you have.
- Holter monitoring. Also known as an ambulatory monitor, a Holter monitor records your heart rhythms for an entire 24-hour period. Wires from electrodes on your chest go to a battery-operated recording device carried in your pocket or worn on a belt or shoulder strap.
While you're wearing the monitor, you'll keep a diary of your activities and symptoms. Your doctor will compare the diary with the electrical recordings to try to figure out the cause of your symptoms. - Echocardiogram. This noninvasive test uses harmless sound waves that allow your doctor to see your heart without making an incision. During the procedure, a small instrument called a transducer is placed on your chest. It collects reflected sound waves (echoes) from your heart and transmits them to a machine that uses the sound wave patterns to compose images of your beating heart on a monitor.
These images show how well your heart is functioning, and recorded pictures allow your doctor to measure the size and thickness of your heart muscle. - Stress test. Some heart problems occur only during exercise. For a stress test, an electrocardiogram is taken before and immediately after walking on a treadmill or riding a stationary bike. In some cases, an echocardiogram or nuclear imaging may be done.
Other types of treadmill exercise tests also can be done to evaluate your heart, including an oxygen consumption test that measures how much oxygen your body is using.
What you can expect
Before the procedure
Surgery to implant the pacemaker is usually performed while you're awake and typically takes a few hours. Before the procedure, you are taken to a special room (called a preparation room or holding area) to start an intravenous (IV) line.Most pacemaker implantations are done using local anesthesia to numb the area of any incisions. You may receive additional IV medication to help you relax. The implantation is done in a room with special X-ray equipment. Your chest is cleaned with an antibacterial soap, and an IV line is placed in your arm on the same side as the pacemaker.
During the procedure
During surgery, one or more flexible, insulated wires (leads, or electrodes) are inserted into a major vein under or near your collarbone and guided to your heart with the help of X-ray images. One end of each wire is secured to the appropriate position in your heart, while the other end is attached to the pulse generator, which is usually implanted under the skin beneath your collarbone.After the procedure
You'll usually stay in the hospital for one day after having a pacemaker implanted. Before you leave, your pacemaker is programmed to fit your particular pacing needs. A return visit is often scheduled to make sure your pacemaker's settings are correct.After that, most pacemakers can be checked remotely using wireless technology. Using your cellphone or radiofrequency signals, your pacemaker transmits and receives information between you and your doctor's office, where your doctor can access the data — including your heart rate and rhythm, how your pacemaker is functioning, and remaining battery life.
Remote transmissions can be made at scheduled intervals or at unscheduled times if your pacemaker sends an alert, or you can send a transmission if you have a concern. Remote technology means fewer trips to the doctor's office, but you'll still need to be seen by your doctor in person for scheduled checkups.
After your procedure to implant your pacemaker, your doctor may recommend that you avoid vigorous exercise or heavy lifting for about a month. You may have some aches and pains near the area where your pacemaker was implanted. These pains can be relieved with over-the-counter medicines, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others), but talk to your doctor before taking any pain relievers.
Special precautions
It's unlikely that your pacemaker would stop working properly because of electrical interference. Still, you'll need to take a few precautions:- Cellphones. It's safe to talk on a cellphone, but avoid placing your cellphone directly over your pacemaker implantation site when the phone is turned on. Although unlikely, your pacemaker could misinterpret the cellphone signal as a heartbeat and withhold pacing, producing symptoms, such as sudden fatigue.
- Security systems. Passing through an airport metal detector won't interfere with your pacemaker, although the metal in it may sound the alarm. But avoid lingering near or leaning against a metal-detection system.
If security personnel insist on using a hand-held metal detector, ask them not to hold the device near your pacemaker any longer than necessary or ask for an alternative form of personal search. To avoid potential problems, carry an ID card stating that you have a pacemaker. - Medical equipment. If a doctor is considering any medical procedure that involves intensive exposure to electromagnetic energy, tell him or her that you have a pacemaker. Such procedures include magnetic resonance imaging, therapeutic radiation for cancer treatment and shock wave lithotripsy, which uses shock waves to break up large kidney stones or gallstones.
If you're having surgery, a procedure to control bleeding (electrocautery) also can interfere with pacemaker function. - Power-generating equipment. Stand at least 2 feet (60 centimeters) from welding equipment, high-voltage transformers or motor-generator systems. If you work around such equipment, your doctor can arrange a test in your workplace to determine whether it affects your pacemaker.
Results
Once your pacemaker is implanted, the battery should last five to 15 years, which is the average battery life. When a pacemaker's battery wears out, the pacemaker's pulse generator is replaced. The leads of your pacemaker can be left in place — though they may need to be replaced eventually — and the procedure to change your pacemaker's battery is often quicker and requires less recovery time than the procedure to first implant your pacemaker.Pacemakers are a standard treatment for many conditions affecting your heart's electrical system. By preventing a slow heart rate, pacemakers can treat symptoms, such as fatigue, lightheadedness and fainting. Because most of today's pacemakers automatically adjust your heart rate to match your level of physical activity, they can allow you to resume a more active lifestyle.
Pacemakers and end-of-life issues
If you have a pacemaker and become terminally ill with a condition unrelated to your heart, such as cancer, it's possible that your pacemaker could prolong the process of dying. Doctors and researchers have varied opinions on turning off a pacemaker in end-of-life situations.Talk to your doctor if you have a pacemaker and are concerned about turning it off. You may also want to talk to family members or another person designated to make medical decisions for you about what you'd like to do in end-of-life care situations.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this disease.Pacemaker care at Mayo Clinic



No comments:
Post a Comment