What are the bundle branches?
Normally, your heart beats in a nice, regular fashion. The heartbeat starts in the upper chambers of the heart in an area called the SA node. The impulse then moves to the AV node. The AV node is an area of tissue that carries the impulse through the Bundle of His and then splits into two wire-like branches (the bundle branches). The branches carry the impulse to the Purkinje fibers, which are located in the muscular walls of the ventricles, and cause them to contract.
What is a bundle branch block?
A bundle branch block means the electrical impulses that control the heartbeat cannot move properly throughout the heart. A block in the branches causes the impulses to travel slower than normal.Diagnosis of bundle branch block
A bundle branch block can be seen on an electrocardiogram (EKG).How LBBB can affect other cardiovascular tests and conditions
Stress testing and heart attack
Left bundle branch block can make it more difficult to diagnose left ventricular hypertrophy (LVH) and ischemia (decreased blood supply to the heart) during exercise stress testing and during a heart attack.
If you have LBBB, make sure your doctor knows about the condition before you have a stress test. You may need additional testing or a different kind of stress test (done with medicine, not exercise).
You should also carry a copy of your EKG with you.
If you think you are having a heart attack, be sure to tell your doctor or nurse that you have LBBB and give them the copy of the EKG. This will help them see changes in your heart.
If you have signs of LVH, your doctor will use an echocardiogram to diagnose the condition.
Symptoms
In most people, bundle branch block doesn't cause any symptoms. Sometimes, people with the condition don't even know they have a bundle branch block.
For those people who do have signs and symptoms, they may include:
- Fainting (syncope)
- Feeling as if you're going to faint (presyncope)
Causes
Normally, electrical impulses within your heart's muscle signal it to beat (contract). These impulses travel along a pathway, including the right and the left bundles. If one or both of these branch bundles become damaged — due to a heart attack, for example — this change can block the electrical impulses and cause your heart to beat abnormally.
The underlying cause for bundle branch blocks may differ depending on whether the left or right bundle branch is affected. It's also possible that this condition can occur without any known underlying cause. Specific causes may include:
Left bundle branch block
- Heart disease
- Thickened, stiffened or weakened heart muscle (cardiomyopathy)
- A viral or bacterial infection of the heart muscle (myocarditis)
- High blood pressure (hypertension)
Right bundle branch block
- A heart abnormality that's present at birth (congenital) — such as atrial septal defect, a hole in the wall separating the upper chambers of the heart
- A heart attack (myocardial infarction)
- A viral or bacterial infection of the heart muscle (myocarditis)
- High blood pressure (hypertension)
- A blood clot in the lungs (pulmonary embolism)
Risk factors
Risk factors for bundle branch block include:- Increasing age. Bundle branch block is more common in older adults than in people who are middle-aged.
- Underlying health problems. People who have high blood pressure or heart disease are more likely to have bundle branch block than people without those conditions.
Complications
The main complication of bundle branch block is a slow heart rate, which can sometimes cause fainting.People who have a heart attack and develop a bundle branch block have a higher chance of complications, including sudden cardiac death, than do people who have heart attacks and don't develop a bundle branch block.
Because bundle branch block affects the electrical activity of your heart, it can sometimes complicate the accurate diagnosis of other heart conditions, especially heart attacks, and lead to delays in proper management of those problems
Diagnosis
Tests that may be used to diagnose a bundle branch block or the underlying problem causing it include:- Electrocardiogram. An electrocardiogram records the electrical impulses in your heart through wires attached to the skin on your chest and other locations on your body. Abnormalities may indicate the presence of bundle branch block, as well as which side is being affected.
- Echocardiogram. An echocardiogram can be used to pinpoint an underlying condition that caused the bundle branch block. This test uses sound waves to produce images of the heart, allowing your doctor to see your heart in motion.
An echocardiogram provides detailed images of the heart's structure and shows the thickness of your heart muscle and whether your heart valves are moving normally
Right bundle branch block (RBBB)
Right bundle branch block (RBBB) is very common, and the risk of developing the condition increases with age. Once your doctor sees RBBB on an EKG, the next step is to see if you have underlying heart disease.If you do not have other heart disease, symptoms of heart disease, or other blocks in your electrical conduction system, no treatment is necessary.
If you have RBBB and another heart condition, such as heart attack or heart failure; dizziness or fainting; or other blocks in your electrical system, you will be treated for the heart disease. You may need a pacemaker if you have symptoms or another heart block.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
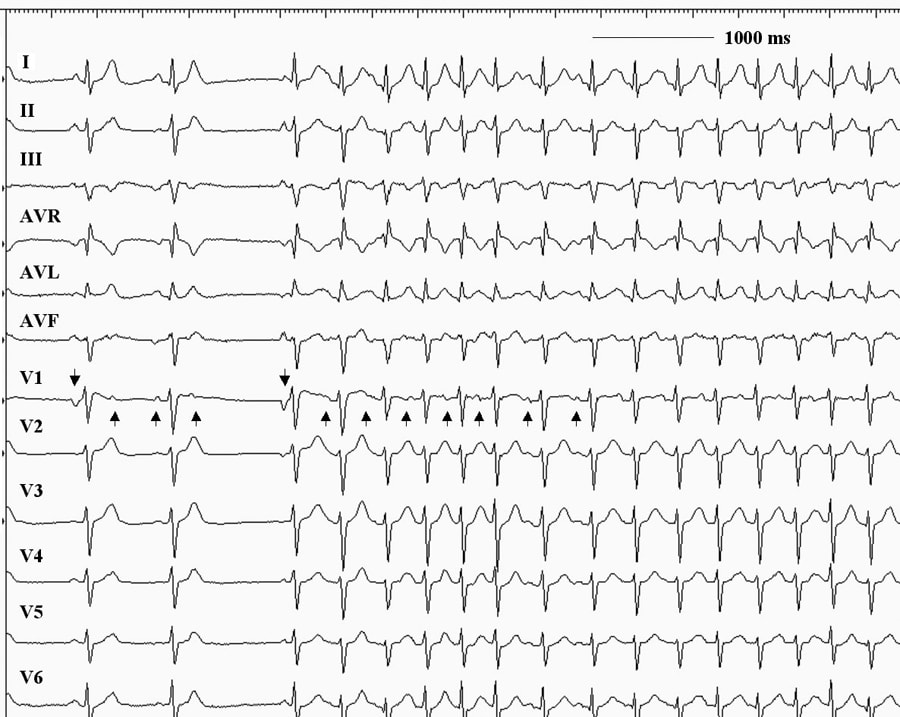
In right bundle branch block, the right ventricle is activated via cell-to-cell transmission of the action potential. This is illustrated in the following animation:
Notice the delay in the time of right ventricular depolarization. This means that the right ventricle is activated after the left ventricle (which is depolarizing normally) and therefore contracts a "split second" after the left ventricle. Mechanically, this difference doesn't greatly influence the performance of the heart. However, it does produce some characteristic changes in the ECG.Electrocardiographic changes in RBBB. As you might be able to guess from the animation, because the depolarization of the ventricle has been altered, the changes show up in the QRS complex and the T wave. The following pictures illustrate right bundle branch block in different leads.
 |
 |
 |
Appearance of three different leads in RBBB: From top to bottom: Lead I, Lead V1 and Lead V6. Due to the RBBB, the right ventricle is depolarizing after the left ventricle. In all three leads, there is a prolongation of the QRS complex due to the blockade. In leads I and V6 (which "see" the left ventricle best), the delayed depolarization of the right ventricle produces a late, negative going wave (S wave) that is very broad (there is no point to the wave) and prolonged. In lead V1 (which has a good view of the right ventricle, the delay in depolarizing the right ventricle leads to the aptly-named "bunny ears"- the QRS complex is composed of an initial positive wave (the R wave), followed by a negative deflection (the S wave) produced when the left ventricle depolarizes, and then a second positive wave (called R' (spoken "R prime")) as the right ventricle finally depolarizes. Because the normal conduction pathway was not followed for depolarization, the process of repolarization does not occur in the normal sequence leading to abnormalities in the T wave (seen best in V1).
|
Summary of electrocardiographic changes in RBBB:
Left bundle branch block (LBBB)
Left bundle branch block (LBBB) is less common than RBBB. As with RBBB, the risk of developing the condition increases with age. Once your doctor sees LBBB on an EKG, the next step is to see if you have underlying heart disease.
If you do not have other heart disease, symptoms of heart disease, or other blocks in your electrical conduction system, no treatment is necessary.
If you have another heart condition, such as hypertension, coronary artery disease or heart attack, myocarditis or heart failure; dizziness, fainting or chest pain; or another block in your electrical system, you will be treated for the heart disease. You may need a pacemaker if you have another type of heart block or have symptoms of heart block.
Left Bundle branch block (LBBB) is very similar to right bundle branch block, as the following animation illustrates.
As with the RBBB, the major change is that the left ventricle is now depolarized due to the spread of the action potential via cell-to-cell conduction. This results in the left ventricle depolarizes (and therefore contracting) a "split-second" after the right ventricle does. As with RBBB, the mechanical effects of this on the heart are minimal.Electrocardiographic changes in LBBB:The following pictures illustrate left bundle branch block as seen in three different leads:
 |
 |
 |
The appearance of LBBB in three different leads: As with right bundle branch block, the major change is in the shape and duration of the QRS complex (since it is ventricular depolarization that has been altered). All of the leads show a prolonged QRS complex due to the time it takes the left ventricle to depolarize. Leads I and V6 record long R waves (lead I shows a small initial R wave (you might be mistaking it for a P wave) and a larger R' leading to a somewhat odd pair of "bunny ears") because the depolarization is heading "at" the lead for a prolonged period of time as the ventricle depolarizes. Lead V1 (on the right side of the sternum sees an initial very small positive wave as the faster right ventricle depolarizes, followed by a prolonged S wave produced by the left ventricular depolarization (note that the S wave also has two peaks - an inverted pair of "bunny ears").
|
Summary of electrocardiographic changes in LBBB:
Treatment
Most people with bundle branch block are symptom-free and don't need treatment.
However, if you have an underlying heart condition causing bundle branch block, treatment of the underlying condition is recommended. Treatment of underlying conditions may involve using medications to reduce high blood pressure or lessen the effects of heart failure, or the use of a coronary angioplasty to open up the artery leading to your heart.
Additionally, depending on your symptoms and whether you have other heart problems, your doctor might also recommend:
- A pacemaker. For some people with bundle branch block and a history of fainting, doctors may recommend implanting a pacemaker. A pacemaker is a compact device implanted under the skin of your upper chest (internal pacemaker) with two wires that connect to the right side of your heart. The pacemaker provides electrical impulses when needed to keep your heart beating regularly.
- Cardiac resynchronization. Also known as biventricular pacing, this procedure is similar to having a pacemaker implanted. However, in cardiac resynchronization, there's a third wire that's connected to the left side of the heart so the device can keep both sides in proper rhythm.